Bob Mackin
Almost two-thirds of British Columbia’s pandemic supplies were never replenished before the novel coronavirus hit the West Coast.
A supply chain memo from the Provincial Health Services Authority, obtained by theBreaker.news under the freedom of information law and shared with CTV News Vancouver, shows that medical equipment stockpiles totalled more than $5.7 million in July 2013.

3M N95 mask
But, by January 2020, they had dwindled to $2.07 million.
Supplies range from syringes, needles and bandages to surgical masks, N95 respirators, gloves, eye goggles, gowns and hand sanitizer. The briefing note quantified the inventory by dollar value, rather than units.
Over the course of six-and-a-half years, almost $2.76 million of supplies owned by B.C.’s five regional health authorities had expired, become obsolete or been donated to anti-Ebola efforts in Africa, while $896,000 of goods had been absorbed into working inventory.
“Most of the expired/donated inventory was not replaced resulting in the current lower level of pandemic supplies,” said the Feb. 13 document, submitted by Melinda Mui, the interim vice-president of PHSA’s supply chain department, to a leadership council meeting.
“Health authorities’ pandemic supply levels have dwindled or been eliminated on many items across the province. Should a widespread pandemic occur in B.C., the current level of pandemic supplies will likely not meet B.C.’s requirements which may lead to public safety risk.”
The agency that spends $2 billion a year on medical supplies for B.C. hospitals and ambulances recommended a centralized provincial pandemic supply chain and plan to return stock to 2013 levels.
Less than a month after Mui’s document, the World Health Organization declared COVID-19 a pandemic on March 11.
“There wasn’t really pandemic preparedness going on there,” B.C. Nurses Union president Christine Sorenson said in an interview with CTV News Vancouver reporter Jon Woodward.
Sorenson said personal protective equipment scarcity is one of the biggest concerns for nurses. She said 100 have filed WorkSafeBC claims due to infection in the workplace.
She agreed it was reasonable, for legal reasons, to get rid of supplies that expired or were no longer manufacturer-approved. But that does not excuse complacent officials, who should have maintained stock while avoiding financial loss.
“What should have been taking place is replacement,” Sorenson said. “There should have been a normal sort of turnover of personal protective equipment, supplies.”
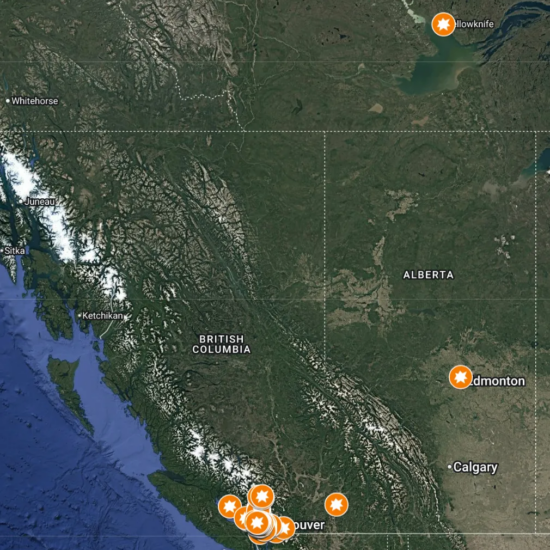
The only health authority with more supplies in 2020 than 2013 was Vancouver Island Health, which had $416,000 versus $375,000 in 2013.
Interior Health’s stockpile value had shrunk from $435,000 to $0 over seven years. Northern Health had just $15,768 remaining. Back in 2013, it had $377,000.

Melinda Mui of PHSA
Vancouver Coastal Health’s stockpile dropped $1 million to $426,000. Fraser Health had $611,855 on hand, down from $1.56 million in July 2013.
Another document acknowledged the risk of each health authority managing its own stock.
“This individual approach leads to an inconsistent approach to managing these critical supplies as they are not currently under centralized direction nor consistent,” according to a Feb. 4 briefing note.
Titled “Health Authority Owned Pandemic Inventory for British Columbia,” it stated centralized supply management would allow the province to reduce costs associated with waste and obsolescence.
Feb. 4 was the week after B.C. announced its first confirmed case of 2019-nCoV. A person who had travelled from Wuhan, China tested positive on Jan. 27 in the Vancouver Coastal Health region.
Even with a way forward, PPE usage rates were reaching beyond historical norms. A February 27 inventory report showed that Northern Health had no supplies of four surgical mask types and only one day’s supply of another. Island Health was out of six surgical mask types and down to a month’s supply of two N95 mask types. The federal government came to the rescue for B.C. and other provinces in March when it chartered CargoJet to bring emergency plane loads of PPE back to Canada from Shanghai.
The stockpiles were originally built under the BC Liberal government. By January 2020, the NDP had been in power for two-and-a-half years. At a July 14 news conference, Health Minister Adrian Dix said B.C. now has adequate PPE on hand as hospitals work to clear the massive backlog of delayed surgeries.
Provincial Health Officer Dr. Bonnie Henry said during the same session that officials conducted a “rapid inventory” in January.
“We never had a shortage,” Henry said. “We did have to keep it managed centrally so there wasn’t hoarding in certain areas. We had a dramatic increase of respirators and masks related primarily to people’s concerns about being exposed. We don’t want to be in that position again. This has made it every clear how challenging it is.”

B.C. Nurses Union president Christine Sorenson
Henry offered conflicting messages four months ago.
On March 23, she said she was unaware of PPE shortages in B.C.
Just two days later, on March 25, a 180-degree pivot: Henry revealed that hospitals were “going through way more personal protective equipment than we expected, so we are on a tenuous level.”
Dr. Roland Orfaly, CEO of the B.C. Anesthesiologists Society, told theBreaker.news that the PPE supply challenge would have been disastrous for his members and patients had the virus spread in B.C. like it did in Quebec.
“It was anesthesiologists who were putting themselves right there, inches from the face of a COVID patient when they were most ill and most infectious,” Orfaly said. “We could be unknowingly intubating a COVID patient for surgery. So having the appropriate type and amount of PPE available is absolutely critical, not just for our safety as anesthesiologists, but for the entire team of healthcare workers around us.”
Global shortage was preventable
The first of the two PHSA briefing notes came three days before the head of the World Health Organization made an alarming announcement at a news conference.
On Feb. 7, Dr. Tedros Adhanom Ghebreyesus warned of a global PPE crisis. Demand had skyrocketed 100 times higher than normal and prices were up to 20 times more expensive.
“This situation has been exacerbated by widespread, inappropriate use of PPE outside patient care. As a result, there are now depleted stockpiles and backlogs of four to six months,” Adhanom said. “Global stocks of masks and respirators are now insufficient to meet the needs of WHO and our partners.”
Medication, supplies and equipment are provincial and territorial responsibilities. The federal government maintains a National Emergency Strategic Stockpile, but that is for provinces to request in emergencies when their own resources are not enough. It is from that inventory that China received a 16-tonne donation in early February, sparking a firestorm of controversy as Canada’s healthcare system began to run out.

Dr. Bonnie Henry (left) and Health Minister Adrian Dix (Mackin)
B.C. built its stockpile after a watershed 2006 report from a committee of top officials, including Dr. Theresa Tam, called Canadian Pandemic Influenza Plan for the Health Sector.
Dr. Danuta Skowronski represented the B.C. Centre for Disease Control, where Henry worked. Henry and Vancouver Coastal Health’s Dr. Patty Daly were involved in subcommittees.
The document warned that a pandemic would likely result in supply shortages and that Canadian governments should not rely heavily on outside assistance. Interrupted transportation lines, lack of inventory and embargoes would complicate procurement.
“Provinces/territories and local health authorities may wish to review the possibility of rotating stockpiles of critical supplies for health care facilities within their own jurisdictions,” the report said.
Governments got another reminder last fall. The 2019 annual report of the WHO’s Global Preparedness Monitoring Board Annual said pandemics from natural pathogens or disease-causing microorganisms from a laboratory posed a major threat. Johns Hopkins University in Baltimore hosted the Event 201 pandemic simulation last November. The table top exercise concluded scarcity of medical supplies was a major weakness.
Two months after the PHSA stockpile report, theBreaker.news revealed how desperate the B.C. government had become.
Mui went to the People’s Republic of China consulate to accept a donation of 56 boxes of PPE from Guangdong province, the week after Premier John Horgan spoke to China’s ambassador to Canada, Cong Peiwu.
Staff in government offices across B.C. received an April 7 memo from Ministry of Health assistant deputy minister Philip Twyford. While bureaucrats were working from home, Twyford wrote that staff went hunting for unused N95 masks in earthquake kits at ministry and agency locations across B.C.
“This was a cross-government effort which provided thousands of masks to front-line health workers,” Twyford wrote in an email obtained by theBreaker.news. “Facilities staff went to each workspace and removed the earthquake kits to check for masks. As a result, some workspaces may have been slightly disturbed when the masks were retrieved. Staff placed the earthquake kits on the floor, and did not reattach them to desks and other surfaces, so we can replenish the kits when a supply is available for this purpose.”
Said anesthesiologist Orfaly: “It’s concerning that there may have been a shortage of PPE going into the pandemic earlier this year. And certainly concerning that if there is a second wave coming up. We need to have enough supplies available.”
theBreaker.news originally sought the documents on April 14, but that was during a two-month period in which Information and Privacy Commissioner Michael McEvoy granted B.C. public bodies a temporary holiday from disclosing records under the FOI law. The PHSA records were finally delivered July 9.
Support theBreaker.news for as low as $2 a month on Patreon. Find out how. Click here.